Abstract
Background: For transplant-ineligible patients with newly diagnosed multiple myeloma (NDMM), the only category 1 regimens recommended by the National Comprehensive Cancer Network (NCCN) are lenalidomide and dexamethasone (Rd)-based, including triplet therapy with lenalidomide, bortezomib, and dexamethasone (RVd) (NCCN Myeloma v4.2018). Other doublet regimens, such as bortezomib and dexamethasone (Vd), are still a first-line option for patients with NDMM, especially for those who are elderly and/or frail. However, the latter population is either excluded or markedly underrepresented in clinical trials. Using an electronic health records (EHRs) database, we compared outcomes when either RVd or Vd were used in the treatment of transplant-ineligible patients with NDMM in a real-world practice setting, after adjusting for baseline demographic and clinical differences between the two cohorts.
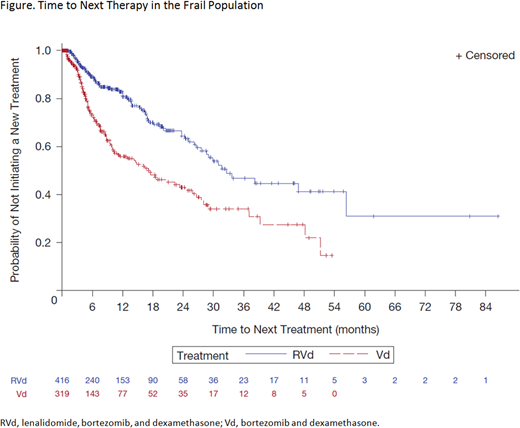
Methods: A retrospective observational study of patients with NDMM was conducted using EHRs from a nationally representative database (Flatiron Health). The Flatiron Network database is an enhanced oncology EHR database of patients treated at 265 clinics throughout the USA. Patients diagnosed with multiple myeloma, ICD-9 (203.0x) or ICD-10 (C90.xx), between January 2011 and May 2018 who were treated with RVd or Vd and did not undergo stem cell transplantation were included in the analysis. The primary comparison was time to next therapy (TTNT) in the overall population and in a subset of frail patients, as determined by a composite score based on age, Eastern Cooperative Oncology Group performance status (ECOG PS) score, and Charlson Comorbidity Index (CCI). Data regarding overall and progression-free survival (PFS) were limited as patient data prior to adoption of the Flatiron Network database were incomplete. Treatment-free interval (TFI) for patients who initiated a second-line therapy was defined as time from start of first-line to start of second-line therapy minus the duration of therapy (DOT). The Kaplan-Meier and Cox proportional hazard methods were used to calculate TTNT after adjusting for differences in patient baseline demographic and clinical characteristics.
Results: Of the 8,470 transplant-ineligible patients with NDMM in the database, 2,369 were treated with either RVd (n = 1,309) or Vd (n = 1,060) and met the criteria for inclusion in this analysis. Patients treated with Vd were more likely to be older (median age 75 vs 70 years; P < 0.0001), frail (76.3% vs 65.4%; P = 0.0002), have creatinine clearance < 30 mL/min (23.9% vs 10.7%, P < 0.0001), have a higher ECOG PS score (P = 0.0031), and have International Staging System stage III disease (45.1% vs 28.8%; P < 0.0001). There were no significant differences in baseline neutropenia, anemia, or thrombocytopenia, or in median CCI. The proportion of patients with high-risk cytogenetics was lower in the Vd group (19.7% vs 26.0%; P < 0.0001).
The mean DOT was longer for RVd (11.4 ± standard deviation [SD] 13.3 months) than for Vd (7.7 ± SD 9.7 months). However, the median adjusted TTNT was significantly longer with RVd than Vd (40.9 vs 14.8 months; hazard ratio [HR] 0.43; 95% confidence interval [CI] 0.33-0.55; P < 0.0001). The proportion of patients initiating a new treatment was lower in the RVd group (24.8% vs 40.6%; P < 0.0001). Among those who initiated a second-line therapy, the mean TFI for RVd compared with Vd was 42.6 versus 39.3 days, respectively (P = 0.2214).
Among the 735 frail patients (416 RVd and 319 Vd), the median TTNT was significantly longer with RVd (32.6 vs 17.1 months; HR 0.40; 95% CI 0.29-0.54; P < 0.0001; Figure). Similar to the overall population, there were no significant differences in TFI (54.9 vs 29.6 days, P = 0.2598) and a significantly higher proportion of Vd patients initiated a new treatment (22.1% vs 36.4%; P < 0.001).
Conclusions: In this real-world practice setting where PFS cannot be measured directly, triplet therapy with RVd significantly prolonged TTNT compared with Vd by 26.1 months in the overall patient population, and by 15.5 months in frail transplant-ineligible patients with NDMM.
Chari:Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Seattle Genetics: Membership on an entity's Board of Directors or advisory committees; Pharmacyclics: Research Funding; Amgen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Takeda: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Adaptive Biotechnology: Membership on an entity's Board of Directors or advisory committees; The Binding Site: Consultancy; Array Biopharma: Research Funding; Bristol Myers Squibb: Consultancy. Ung:Celgene Corporation: Employment, Equity Ownership. Tian:Celgene Corporation: Employment. Agarwal:Celgene Corporation: Employment, Equity Ownership. Parikh:Celgene Corporation: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal